Living with diabetes can be challenging, but with the right knowledge and tools, it’s possible to manage the condition effectively. One of the most critical aspects of diabetes management is monitoring your blood glucose levels. This process helps you understand how your body responds to food, exercise, medication, and other factors, allowing you to make informed decisions about your health. In this comprehensive guide, we’ll explore essential tips for glucose monitoring, including how to choose the right device, when to test, and how to interpret your results. If you start searching the options below, you can find the best deals for you.
Understanding the Importance of Glucose Monitoring
Glucose monitoring is a vital part of managing diabetes. Regular checks of your blood sugar levels can help you avoid the dangers of both hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar). Both conditions can lead to serious health complications if not addressed promptly.
Moreover, glucose monitoring can help you understand how different factors affect your blood sugar levels. For instance, you might notice that certain foods cause a spike in your glucose, while physical activity tends to lower it. This knowledge can guide your decisions about diet, exercise, and medication.
Choosing the Right Glucose Monitor
There are many glucose monitors available on the market, and the best one for you depends on your individual needs and circumstances. Some people prefer traditional finger-stick devices, while others opt for continuous glucose monitors (CGMs) that provide real-time readings.
CGMs, on the other hand, use a sensor inserted under the skin to measure glucose in your tissue fluid. They provide continuous readings and can alert you if your glucose levels are too high or too low. However, they are more expensive than finger-stick devices and may not be covered by all insurance plans.
Type 1 and Type 2 Diabetes
People with type 1 diabetes often need to test their blood sugar levels several times a day. This includes before meals and snacks, before and after exercise, before bed, and sometimes during the night. They may also need to test more frequently if they are ill or under stress.
For people with type 2 diabetes, the testing schedule can vary widely. Some people may need to test only once or twice a day, while others may need to test more often. Your doctor can provide specific recommendations based on your treatment plan and how well your diabetes is controlled.
Interpreting Your Results
Generally, a normal fasting blood sugar level for people without diabetes is between 70 and 100 mg/dL. For people with diabetes, the American Diabetes Association recommends a target fasting blood sugar level of 80 to 130 mg/dL. However, your target range may be different depending on your age, how long you’ve had diabetes, and other health conditions.
If your glucose readings are consistently above or below your target range, it’s important to talk to your doctor. They may need to adjust your treatment plan to help you better control your blood sugar levels.
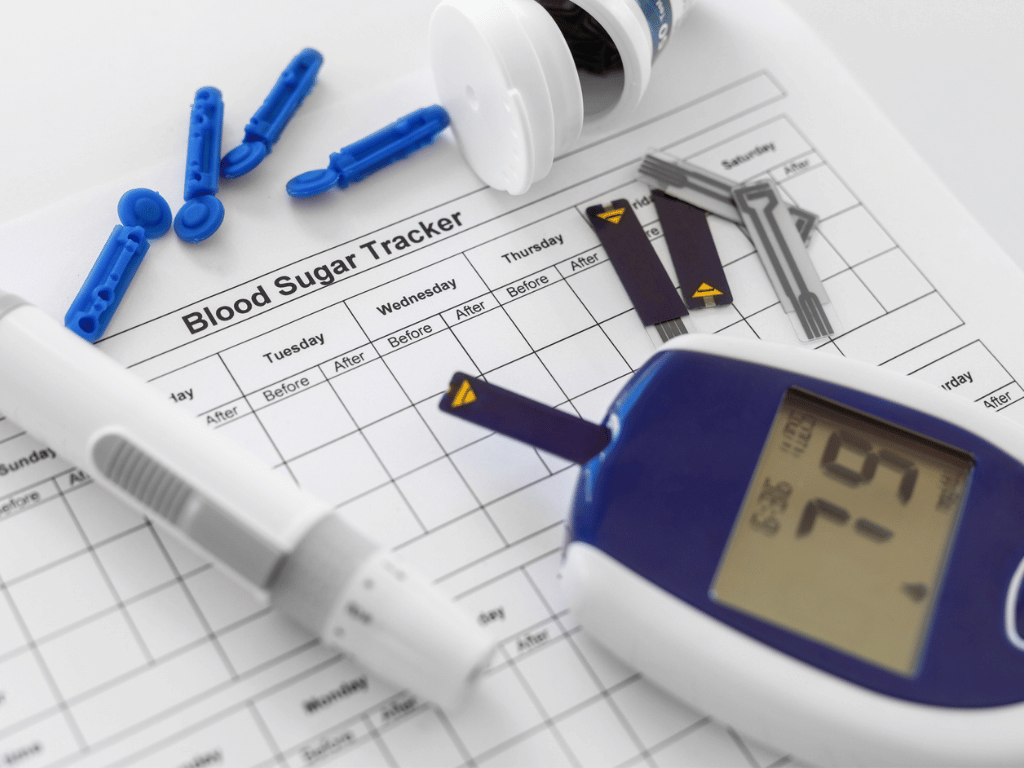
Keeping a Record of Your Readings
Keeping a record of your glucose readings can be incredibly helpful in managing your diabetes. This record can help you and your healthcare team see patterns and trends in your blood sugar levels, which can inform changes to your treatment plan.
Along with your glucose readings, it can be helpful to note the time of each test, what you ate, any physical activity you did, and any unusual events, such as illness or stress. This information can provide valuable context for understanding your blood sugar patterns.
Remember, the best glucose monitoring routine is the one that works for you. It should fit your lifestyle, meet your healthcare needs, and help you feel confident in managing your diabetes. Always consult with your healthcare provider for personalized advice and support.