Ulcerative colitis (UC) is a chronic condition that affects the large intestine, leading to inflammation and ulcers in the digestive tract. Living with UC can be challenging, but with the right diet and nutrition, you can manage your symptoms and maintain a healthy gut. This guide will provide you with valuable tips and insights on how to navigate diet and nutrition with UC. If you start searching the options below, you can find the best deals for you.
Understanding Ulcerative Colitis
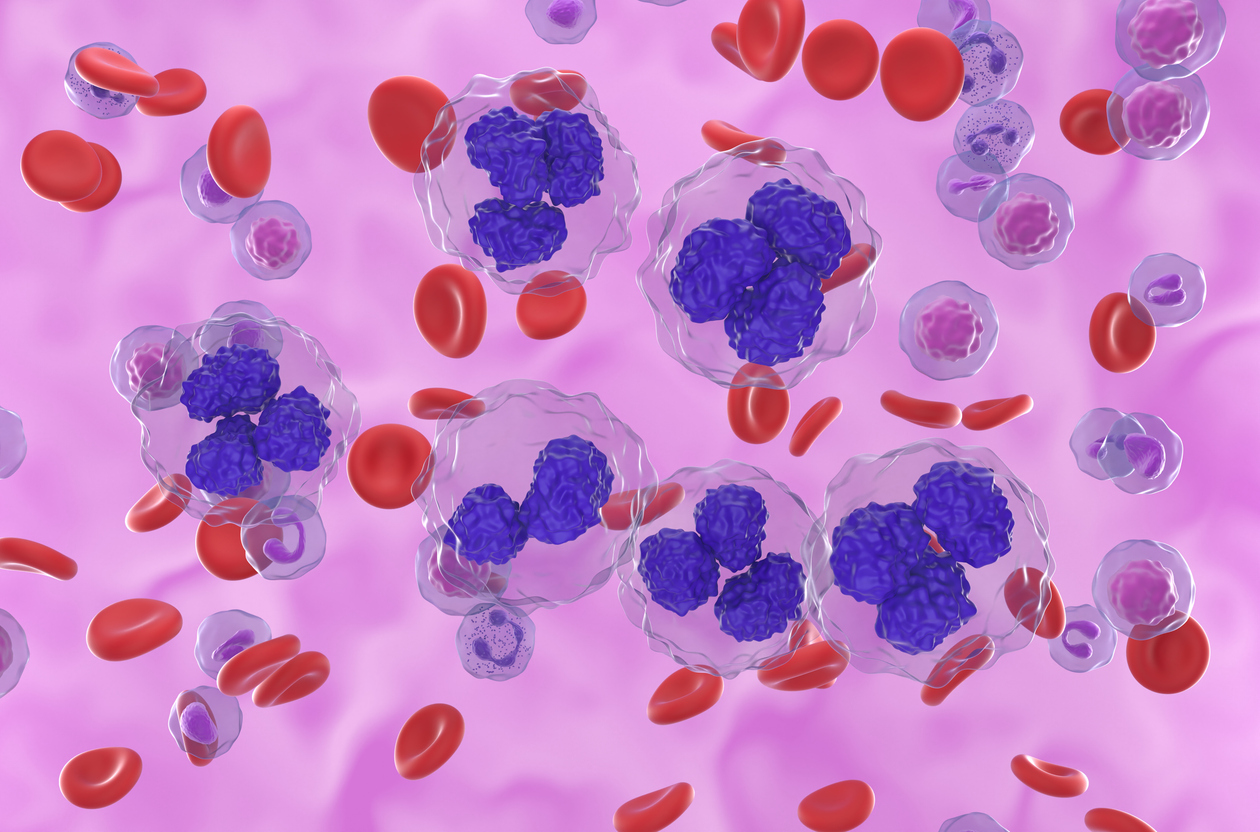
Before delving into the dietary aspects, it’s crucial to understand what UC is. Ulcerative colitis is a type of inflammatory bowel disease (IBD) that primarily affects the innermost lining of your colon (large intestine) and rectum. Symptoms usually develop over time, rather than suddenly. UC can be debilitating and can sometimes lead to life-threatening complications.
While UC has no known cure, treatment can greatly reduce signs and symptoms of the disease and even bring about long-term remission. And that’s where diet and nutrition come into play. Although UC is not caused by the foods you eat, certain types of food can aggravate its symptoms. Therefore, understanding what to eat and what to avoid can help you manage the condition.
The Role of Diet in Managing UC
While diet doesn’t cause UC, it plays a significant role in managing its symptoms. Certain foods might exacerbate your symptoms, while others can help reduce inflammation and promote gut health. It’s important to note that everyone is different, and what works for one person might not work for another. Therefore, it’s crucial to pay attention to your body and identify which foods trigger your symptoms.
Generally, a balanced diet is recommended for people with UC. This means eating a variety of foods that provide all the necessary nutrients your body needs. However, during a flare-up, you might need to adjust your diet to help manage your symptoms.
What to Eat
Foods that are easy to digest and anti-inflammatory can help manage UC symptoms. These include lean proteins, such as chicken, turkey, and fish; cooked vegetables that are easy to digest, like carrots, peas, and potatoes; and low-fiber fruits, such as bananas and melons.
Probiotics, found in foods like yogurt and sauerkraut, can also be beneficial. They help restore the balance of bacteria in your gut, which can be disrupted by UC. Additionally, it’s important to stay hydrated by drinking plenty of water, as UC can lead to dehydration.
What to Avoid
On the other hand, certain foods can trigger UC symptoms. These include high-fiber foods, such as whole grains and raw vegetables; spicy foods; caffeinated and alcoholic beverages; and dairy products, if you’re lactose intolerant.
Again, it’s important to note that everyone is different. What triggers one person’s symptoms might not affect another. Therefore, it’s crucial to keep a food diary to track what you eat and how it affects your symptoms.
Creating a UC-Friendly Diet Plan
Creating a diet plan that works for you is a crucial part of managing UC. This involves identifying your trigger foods, incorporating UC-friendly foods into your diet, and adjusting your diet during flare-ups.
Working with a dietitian can be very helpful in creating a personalized diet plan. They can provide you with expert advice on what to eat and what to avoid, based on your individual needs and preferences.
Identifying Trigger Foods
The first step in creating a UC-friendly diet plan is identifying your trigger foods. These are foods that cause or worsen your symptoms. To do this, keep a food diary where you record everything you eat and any symptoms you experience. Over time, you’ll be able to see patterns and identify which foods trigger your symptoms.
Incorporating UC-Friendly Foods
Once you’ve identified your trigger foods, the next step is to incorporate more UC-friendly foods into your diet. These are foods that are easy to digest and anti-inflammatory. Again, a dietitian can provide you with a list of these foods and help you create a meal plan that includes them.
Adjusting Your Diet During Flare-Ups
During a flare-up, your gut may be more sensitive, and you may need to adjust your diet accordingly. This might involve eating smaller, more frequent meals; avoiding high-fiber foods; and drinking plenty of water to stay hydrated.
Navigating diet and nutrition with ulcerative colitis can be challenging, but with the right information and support, it’s possible to manage your symptoms and maintain a healthy gut. Remember, everyone is different, and what works for one person might not work for another. Therefore, it’s crucial to listen to your body, identify your trigger foods, and create a diet plan that works for you.
Lastly, don’t hesitate to seek professional help. A dietitian can provide you with expert advice and support, helping you create a personalized diet plan that meets your individual needs and preferences. With the right diet and nutrition, you can live a healthy and fulfilling life with UC.